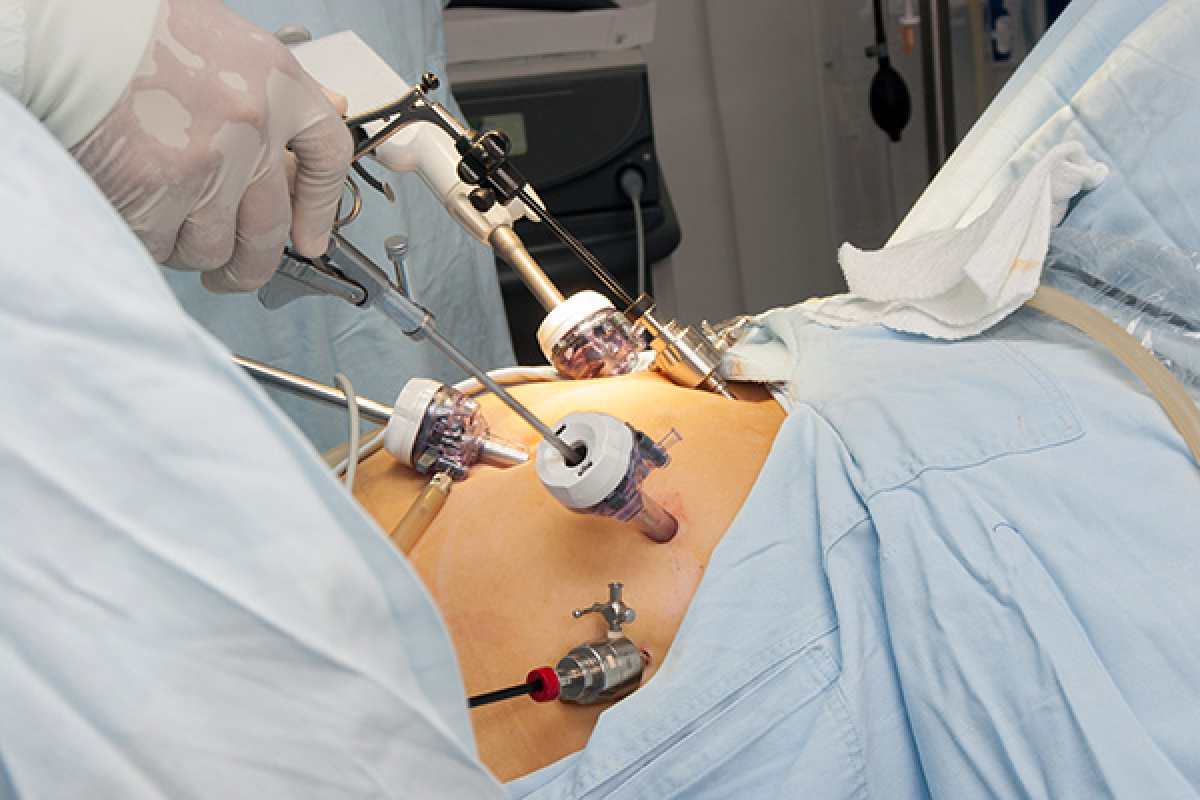
Bariatric Surgery – Embarking on a journey toward significant weight loss is a courageous step, and for many, bariatric surgery is a beacon of hope. It’s a powerful tool against obesity, potentially life-changing. Yet, understanding the risks is just as crucial as recognizing the benefits. Today, we’re diving deep into the realities of bariatric surgery, especially focusing on the times it doesn’t go as planned.
Bariatric surgery is a medical procedure, it’s a life-altering decision aimed at weight loss and managing obesity-related health conditions. Each type offers different approaches and outcomes, from Gastric Bypass to Sleeve Gastrectomy. Let’s explore what these surgeries entail and how they help combat obesity.
Table of Contents
How Often Do Complications Occur?
Bariatric surgery has become increasingly safe, thanks to advances in surgical techniques and better patient care protocols. However, like any major surgery, it does come with its set of risks and potential complications. The frequency of complications varies depending on the type of surgery, the patient’s health status, and the care provided before and after the procedure.
Statistics show that major complications occur in approximately 4% to 6% of bariatric surgery patients. Minor complications, such as nausea and digestive issues, are more common but are often manageable with proper care and medication.
It’s important to note that the mortality rate for bariatric surgery is relatively low, around 0.1% to 0.5%, comparable to the mortality rates of other widely performed surgeries like gallbladder surgery.
The most common complications can be divided into early and late postoperative complications. Early complications, which occur shortly after surgery, include infections, bleeding, and issues related to the surgery itself, such as leaks from the site where the intestines are sewn together.
Late complications can include nutritional deficiencies, gallstones, and long-term gastrointestinal issues like dumping syndrome, which affects how fast food passages from the stomach to the intestines.
Understanding and discussing these risks with a healthcare provider can help make an informed decision about undergoing bariatric surgery.
Major Complications Explored
Some complications, like anastomotic leakage or nutritional deficiencies, can be severe. Knowing about these potential risks and the signs to watch out for post-surgery is important.
Minor Complications Explored
Not all complications are life-threatening, but knowing about the minor ones, such as nausea or scarring, is equally important. Managing these effectively can significantly impact the recovery process.
The journey doesn’t end with the physical transformation. The psychological impact of bariatric surgery is profound, necessitating a support system for mental health throughout this journey.
Factors Influencing Complication Rates
The risk of complications surgery is influenced by several factors, including:
- Patient Factors: Age, overall health, and the presence of obesity-related conditions like diabetes, hypertension, or heart disease can impact the risk of complications. Patients with a higher body mass index (BMI) or those with significant comorbidities may face a higher risk of complications.
- Type of Surgery: Different bariatric procedures carry different risk profiles. For instance, more invasive surgeries like gastric bypass may have a higher risk of complications compared to less invasive options like the gastric sleeve Turkey.
- Surgeon and Hospital Experience: The experience and skill level of the surgeon and the healthcare team, as well as the facility where the surgery is performed, play a crucial role in minimizing risks. High-volume centers and surgeons with extensive bariatric surgery experience tend to have lower complication rates.
- Lifestyle Factors: Postoperative lifestyle choices, including diet, exercise, and adherence to follow-up care, significantly impact the risk of complications and the overall success of the surgery.
Understanding and addressing these factors can help reduce the risk of complications and improve the surgery’s success rate.
Preoperative Measures to Reduce Risks
To minimize the risks associated with bariatric surgery, several preoperative measures are recommended:
- Nutritional Counseling: A thorough nutritional assessment and counseling by a dietitian can help address any deficiencies before surgery and prepare patients for the dietary changes required post-surgery.
- Medical Evaluation: A comprehensive medical evaluation, including lab tests and screenings, can help identify and manage any health issues that may increase the risk of complications.
- Weight Loss: Some patients may be advised to lose a certain amount of weight before surgery to reduce the size of the liver and decrease surgical risk.
- Psychological Evaluation: Understanding the psychological readiness of a patient for surgery and the following lifestyle changes is crucial. This can include assessments and counseling to address eating disorders or other mental health conditions.
- Smoking Cessation: Patients who smoke are advised to quit before surgery, as smoking can increase the risk of complications and slow the healing process.
- Education: Providing patients with detailed information about the surgery, expected outcomes, potential risks, and lifestyle changes required post-surgery is vital for informed decision-making and adherence to postoperative guidelines.
By taking these preoperative steps, patients can significantly reduce their risk of complications and set the stage for a successful recovery and long-term weight management.
Embarking on a bariatric surgery journey is a significant decision. With information, support, and a clear understanding of the risks and rewards, you can make an informed choice that best suits your health and wellness goals. Discover how Luna Clinic can support your weight loss journey and post-surgery recovery.